Researcher Mandana Vahabi works with marginalized people who have a cervix to determine effectiveness of HPV self-sample testing
Pap tests have been the most common method of cervical cancer screening for the past few decades, but they can be an uncomfortable and sometimes traumatic experience for many people with a cervix. HPV self-sampling has arrived as new testing method that offers women and people with a cervix, more control and comfort over their own reproductive health.
A recent study led by Professor Mandana Vahabi of the Lawrence Bloomberg Faculty of Nursing, has found that women who are under-screened for cervical cancer, such as sex workers, those who have a history of incarceration, or who have experienced sexual violence, benefitted from using HPV self-sampling kits and found them easy to use. As a result of the study, one-third of participants were found to have a high-risk strain of human papilloma virus (HPV) following their self-sample and were referred for follow-up testing.
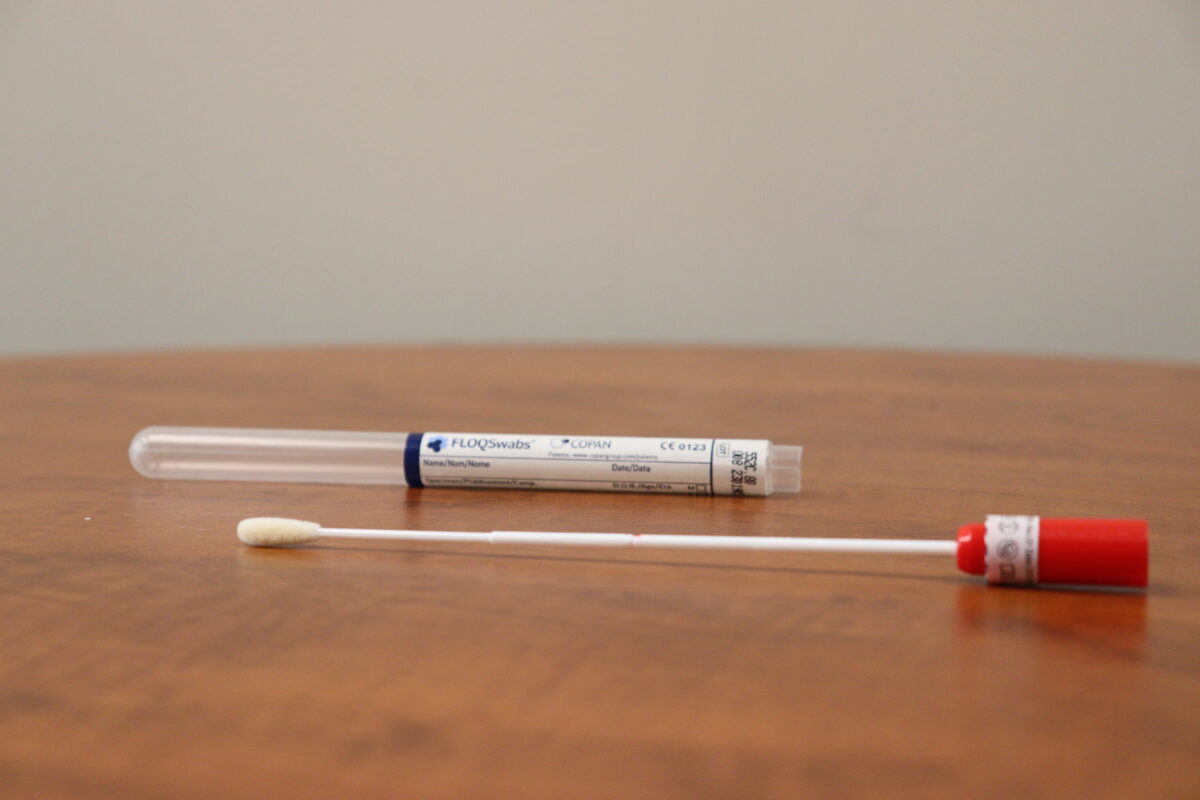
“HPV self sample kits are simple to use and convenient, not that much different from an at-home COVID test,” says Vahabi, who is also the Women’s Health Research Chair at Unity Health. “With this method, individuals can test themselves at a time and place that is convenient for them. They have control in terms of inserting the swab which provides less discomfort than traditional methods. And for many different cultural groups, where modesty is valued, self-sampling reduces stigma and embarrassment.”
Many study participants also shared that they had either never had a pap test, or had chosen not to follow-up on their screening, because of stigma they had faced during their first pap test related to their occupation, lifestyle, or gender identity.
The study was published in the Current Oncology.

What happens if you test positive for HPV?
There are over 100 different strains of the Human Papilloma Virus (HPV) of which four strains are considered high risk for the development of cervical cancer. Vahabi explains that the switch to HPV screening in many different countries and within some provinces in Canada, is intended to get at the root cause of cervical cancer, which is the human papilloma virus and its potential to cause damage to the cervical walls.
Those who test positive for a high-risk strain of HPV, would be asked to undergo a pap test to look for abnormalities in the cervix and early detection Vahabi stresses, is key.
“Once an abnormality is detected we can start an intervention, whether that is laser surgery, cryosurgery (freezing) or removal of damaged tissue to prevent disease progression. This is one of the most important tools we have to save the lives of women,” says Vahabi.
Vahabi has been a staunch advocate for HPV self-sampling kits, particularly because it addresses many of the structural barriers women face in accessing screening including the lack of a primary care physician. She is hopeful that provincial governments will move towards policies that include HPV self-sampling as a method of cervical cancer screening soon.
“Our study showed how stressful it is for a sex worker to seek out screening because they are penalized for what they do, and preached at regarding the risk of their occupation. We are creating a lot of unnecessary fear that prevents them from accessing resources that can save their lives,” says Vahabi.
There are some challenges to scaling up the use of HPV self-sampling. Mistrust of health care providers, and a lack of confidence among participants in conducting the test themselves were some of the key findings from the study, but they were remedied Vahabi says, by sharing appropriate instructions through videos or illustrated pamphlets as well as having nurse practitioners near by to assist if needed.
Raising awareness
January is also cervical cancer awareness month, and Vahabi says that there is still limited knowledge about the risks and symptoms of cervical cancer and HPV.
“Telling people that they are at high risk because of multiple sexual partners is not effective, we need to be explaining that the virus can show up in anyone, and in addition to being vaccinated for HPV, screening is vital to keeping people healthy and informed,” says Vahabi.